
We are now several months into a global pandemic. Daily news is rife with the latest case counts and deaths due to COVID-19, the respiratory disorder caused by a new coronavirus called SARS-CoV-2.
And as I predicted, anxiety is now on the rise. In August, the U.S. Centers for Disease Control published an update to their ongoing assessment of mental health, substance use, and suicidality among U.S. citizens. [1]
The results are not good.
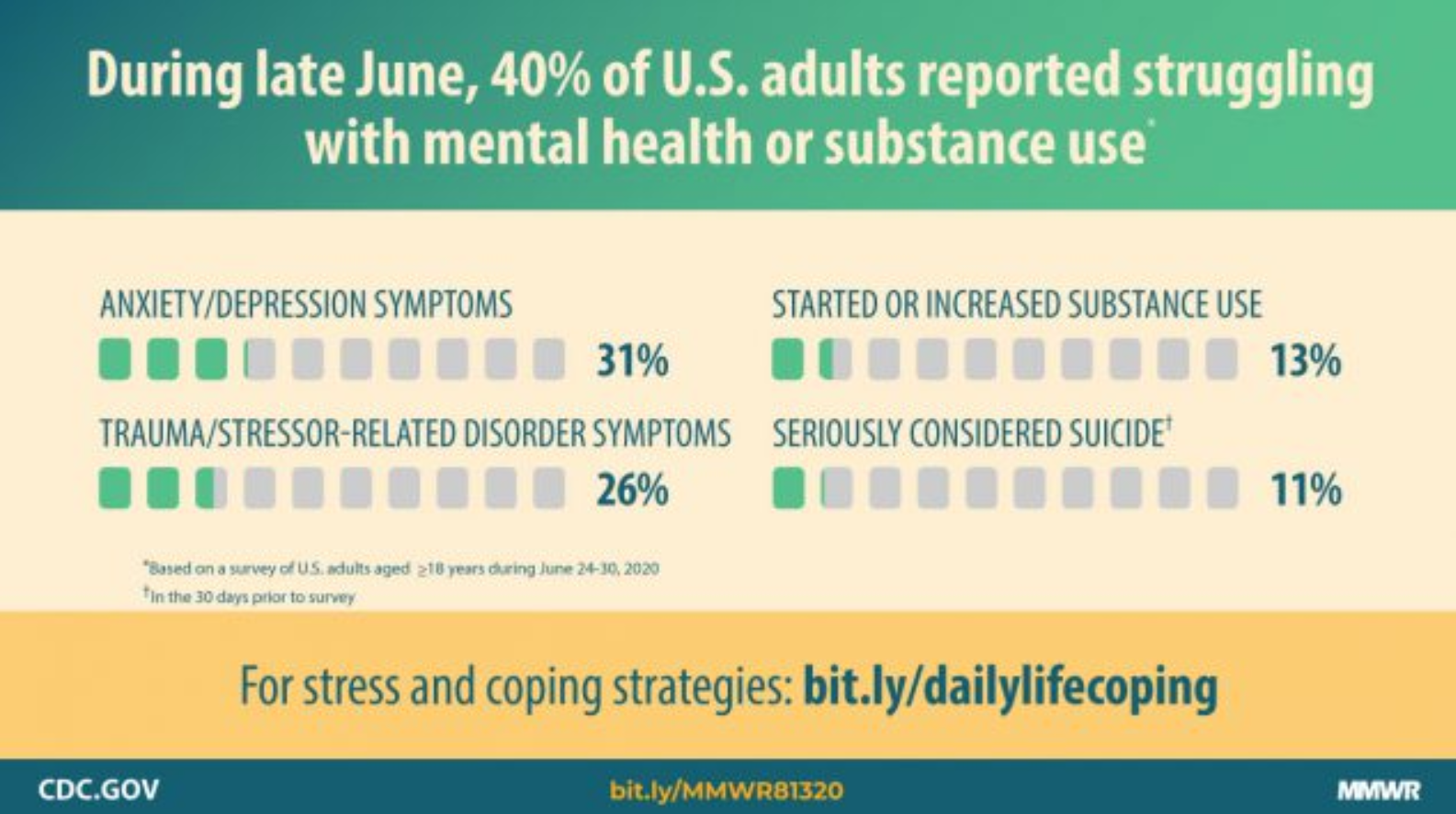
Graphic by Centers for Disease Control (see footnote)
Consider the following:
- Symptoms of anxiety have tripled, going from 8% in 2019 to 26% in 2020;
- Symptoms of depression have quadrupled, going from 6% in 2019 to 24% in 2020;
- Twice as many have had serious thoughts of suicide (11%) compared to 4% in 2018;
- One in 4 have reported symptoms of a trauma disorder due to COVID-19; and
- One in 10 report they have started or increased substance use due to COVID-19.
Younger adults aged 18-24, Hispanic and black persons, essential workers, and unpaid caregivers have borne the brunt of the mental health crisis. They report disproportionately high rates of mental health issues, increased substance use, and thoughts of suicide compared to the rest of us.
I’m starting to feel like a broken record, but let me say once again that it’s never been more important to care for our mental health.
How Has COVID-19 Affected Your Mental Health?
Here are some common symptoms of stress and anxiety:
- Changes in appetite
- Changes sleeping patterns due to upsetting thoughts or nightmares
- Frequent aches and pains, stomach problems, skin rashes
- Worsening of chronic health problems
- Anger or short temper
- Drinking or smoking more
- Trouble thinking or concentrating
- Feeling numb or dreamlike
- Feeling fearful, anxious, depressed
According to a recent poll by the Kaiser Family Foundation, more than half of Americans are suffering from at least one of these symptoms.
In this article, I’ll cover the do’s and don’ts of handling anxiety during COVID-19. But first, let's run through the symptoms we may experience with one or more anxiety disorders.

Photograph by Ian Espinosa on Unsplash
Know the Signs of Anxiety Disorders
Clinical anxiety causes amped up feelings of fear and anxiety. We often use these two terms interchangeably, but psychologically speaking, we fear things in the present and we are anxious about future threats.
There is also a biological difference between the two: fear summons the fight-or-flight response which jump-starts our heart rate, blood pressure, and muscle activity to either fight a threat or get away from it as fast as we can.
By contrast, anxiety is like sitting in the foxhole, waiting for the battle to begin. Our minds and bodies remain clenched in cautious vigilance; we buck and startle at any small movement.
Anxiety disorders feed feelings of fear and anxiety until they loom larger than the threat itself.
There are several types of anxiety disorders, and they often overlap in the same individual. Watch for these warning signs in your loved one:
Generalized Anxiety Disorder (GAD)
- general restlessness; feeling “keyed up”
- easily fatigued
- difficulty concentrating
- irritability
Those with GAD struggle with anxiety almost all the time and about many issues including their health, finances, and relationships. Fear is their constant companion, and they often have the sense the something terrible is about to happen. Their anxiety is so powerful that it often gets in the way of daily life.
Triggers: No real triggers; causes constant or recurrent symptoms
Symptoms:
While anxiety disorders can occur during any stage of life, they often surface early, during adolescence or young adulthood.
Some scientific data suggests that certain anxiety disorders can be inherited through genetics or family predisposition. Most strike about twice as many women as men. If a certain disorder runs in your family, it’s worth monitoring your loved ones extra carefully.
Clinical anxiety locks us into cages of fear, removed from daily life. Sufferers struggle to maintain normal routines at home and work. They may struggle to stay engaged in relationships. They may also suffer other forms of mental illness, like depression. To escape their fear and despair, sufferers may turn to counterproductive and potentially life-threatening solutions like alcohol and illicit drugs.
The good news is, clinical anxiety and depression can be effectively treated using two main approaches: medication and therapy. These both take time and patience to work but can be highly successful when monitored by a qualified healthcare professional.
Buy my latest book
My book, Leaving the Shadowland, describes research-based ways to break the link between the stress we experience and its emotional aftershocks, like depression and anxiety.
Photo by Jairo Alzate on Unsplash
DO’s and DON’Ts for COVID-19 Anxiety
There are many effective ways to help a loved one with their anxiety. Then again, there are some things that may backfire and make a loved one feel even more stressed and anxious.
DON’T constantly reassure them.
I know. This one sounds like it should work. But it often doesn’t, and it may end up making your loved one’s anxiety worse.
To illustrate what I mean, imagine you are going through a stressful time and someone is calling you several times a day “just to check in” and reassure you, “It’s okay, Honey. Everything is going to be okay.”
Some of us would love this. But can you see how the constant queries and assertions may actually plant seeds of doubt in your mind, like, “Why does he/she feel that I need this much reassurance? Maybe I can’t handle what’s going on, after all.”
I want to be careful in how I say this, because reassurance can be a great thing. We just don’t want to repeat ourselves so often and so loudly that we undermine our loved one’s ability to cope. Instead of alleviating his/her stress and anxiety, this will only reinforce those feelings.
DO validate anxious feelings while exploring ways through them.
We should be careful not to downplay, dismiss, invalidate, mock, or reject our loved one’s feelings. Instead, we should listen with patience and empathy, especially during these stressful times.
Validating does not necessarily mean that you agree with your loved one’s feelings. What you are doing is acknowledging the presence of those feelings. You are saying, “I understand how you feel. Everyone gets scared sometimes.”
Once a person feels validated in their feelings, they feel much more confident in taking the next step: finding a way through them. Don’t try to do this for your loved one through excessive reassurance (see above). Instead, walk alongside them, encouraging them and coaching them to find their own solutions. Ask thoughtful, open-ended questions. Practice empathy. Celebrate successes along the way.
Instead of saying, “Everything will be okay,” try saying, “You can get through this. Let’s think together of ways to do that.” The first focuses on external circumstances that may not require any long-lasting emotional strength. But the second focuses on the internal; building up your loved one’s belief in their own strength and resilience.
DON’T overdo media.
I’ve mentioned this one before, but it bears repeating. Don’t overdo media, whether that means news coverage, social media, etc.
I have struggled with this one myself as the United States and the world have grappled with wave after wave of tragedy and trauma. I want to know what’s going on, so I scroll through article after article and one op-ed piece after another.
But there’s a difference between consuming and gorging on media sources. The first may lead to well-informed citizens who engage in local and national causes. The second, I’m convinced, may very well turn us all into media-bloated blobs of frustration and frayed nerves.
DO know and act on the facts.
Which news outlet you choose is completely up to you. For myself, I’m trying to get my COVID-19 facts as close to the scientific sources as I can, for example: the CDC website.
Acting in ignorance is scary. But acting on the facts is calming and empowering.
DON’T hide.
As discussed above, most anxiety disorders cause us to want to run away from normal life. But this is counterproductive in several ways:
- It interferes with our ability to maintain a normal routine. Research shows that a regular, predictable routine is an effective way to reduce anxiety symptoms.
- It keeps us isolated. Social support is also key in reducing feelings of anxiety.
- It doesn’t solve any problems. Running and hiding doesn’t make the problem go away. Nor does it really take away our anxiety.
DO find support.
Need support for your anxiety? There are literally hundreds of support choices out there. Here’s a list of my favorites right now:
- Anxiety and Depression Association of America: Coronavirus Anxiety Tips and Resources
- American Institute of Stress: Stress Management
- Centers for Disease Control: Managing Stress and Anxiety
- American Psychological Association: Anxiety
- American Psychological Association: Stress Management for Leaders
Can I help you in other ways?
See a couple options below for other resources:
Buy my latest book
My book, Leaving the Shadowland, describes research-based ways to break the link between the stress we experience and its emotional aftershocks, like depression and anxiety
Book a coaching call
I also work with business and healthcare leaders who are dealing with stress and overwhelm. If you are struggling with your stress, consider visiting my business website
[1] Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–1057. DOI: http://dx.doi.org/10.15585/mmwr.mm6932a1external icon.
Dr. Pamela Coburn-Litvak has published research articles on exercise and stress in Neuroscience and Neurobiology of Learning and Behavior. Her latest book, Leaving the Shadowland of Stress, Anxiety, and Depression, was published in 2020.
After receiving a Ph.D. in Neurobiology and Behavior from the State University of New York at Stony Brook, she served as both Assistant Professor of Physiology & Pharmacology and Special Assistant to the Vice President for Research Affairs at Loma Linda University in Loma Linda, California. She then joined the Biology department at Andrews University and developed courses in human physiology as well as the neurobiology of mental illness. She also founded Rock @ Science LLC, a company that specializes in health and science education and web development. She co-developed the brain and body physiology segment of the Stress: Beyond Coping seminar with its creator, Dr. William “Skip” MacCarty, DMin.
Dr. Coburn-Litvak currently lives in California with her husband. Their two daughters are mostly grown and attending school elsewhere.
When she’s not studying or teaching about stress, she enjoys stress-relieving activities like puttering around the garden, taking nature walks with her family, knitting, cooking, and reading.


