
I didn’t know what was wrong with me.
Starting in my late teens, I began having extreme bouts of insomnia. I’m a night owl to start with, but sometimes I would find it extra difficult to drop off at night, no matter what I tried.
I would toss and turn through the long night, twisting arms and legs and bedding into a tangle. I was the fly caught in a web of wakefulness, and my alarm clock was the spider with glowing, taunting eyes. Helplessly I would watch it gobble up minutes and then hours, bringing on another bleary day.
The weird thing was, these insomnia episodes always happened at the same time. Twice every year like clockwork, I could count on having a few weeks of sleeplessness.
And – no big surprise – I could also count on dropping into an emotional funk every time. I’d get extra cranky and weepy, binge on comforting carbs, and hope that eventually I’d start sleeping again.
Only later did I get what was going on.

I am among the 5 percent of American adults who struggle with seasonal affective disorder (SAD). SAD is a type of depression that occurs in predictable, seasonal patterns throughout the year.
For reasons we will discuss in a bit, it’s much more common to experience SAD in the late fall/early winter months. But some also experience SAD in the summer.
Apparently, I get to do both. Lucky me.
Since it happens more often in wintertime, SAD is commonly called the “winter blues.” But scientific research says that they are not the same thing at all.
SAD is not as simple as just feeling blue. It is, after all, one form of major depressive disorder (MDD) and can have serious, even life-threatening, results.
In this article, we will explore the difference between SAD and other types of depression. We will see that while there is a lot of overlap between SAD and major depression, SAD also has unique quirks of its own in terms of symptoms, risk factors, and most importantly, treatment options.
Here’s what you need to know.

SAD vs. Depression Symptoms
What they have in common:
As a type of major depression, signs of SAD may include feeling:
- sad or blue
- bored and apathetic
- exhausted
- irritable
- anxious
- fuzzy and unfocused
- hopeless
- worthless
These symptoms may be mild at first but can worsen over time.
Like other forms of depression, SAD can throw normal body functions for a loop by disrupting sleeping and eating patterns. But there are some differences between winter and summer SAD.
Winter SAD symptoms include:
- oversleeping
- eating more than usual, especially high carbohydrate comfort foods
- gaining weight (see previous point!)
- and feeling tired, groggy, or fatigued.
SAD that starts in the late spring or summer months can produce very different symptoms:
- insomnia
- eating less than usual
- losing weight (see previous point)
- and feeling agitated and anxious.
Those with bipolar disorder have depressive episodes intermixed with periods of feverishly high activity or mania. For some bipolar patients, the summer months can bring on manic episodes while the winter can trigger depressive episodes.

Complications of SAD and Depression
Like other forms of depression, SAD can get progressively worse until it disrupts normal life. Depressed and SAD individuals can:
- isolate themselves from friends and family
- drop in school or work performance
- begin to abuse alcohol or other drugs
- experience symptoms of other, overlapping disorders including anxiety or eating disorders
- start thinking or acting on suicidal impulses.
Everyone has “blue” days. This is normal. But if you start feeling blue and droopy for days at a time, please consider seeing a doctor. The Mayo Clinic recommends seeking medical help if your sleep and eating patterns have significantly changed, you start relying on alcohol or other substances for emotional comfort, or you feel hopeless or suicidal.

Causes of SAD, Depression, and the Blues
Researchers think that the winter “blues” are likely tied to the winter holidays because they throw feelings of isolation and loneliness into sharper relief. Such feelings are emotionally stressful.
Stress can also lead to major depression. But there are also other causes:
- medical issues like inflammation and oxidative stress;
- drops in important brain chemicals like serotonin, dopamine, and norepinephrine;
- changes in brain activity which lead to problems in regulating emotion and mood; and
- distorted thought patterns that lead to distorted feelings.
Since SAD is a form of major depression, there is some overlap in its causes. But there are some key differences as well.
It’s important to understand these specific differences because they lead to more specific treatments than those used for other types of depression. SAD causes include:
- drops in important brain chemicals, specifically serotonin. Serotonin is a “feel-good” chemical that helps us deal with stress.
- changes in melatonin levels. Melatonin is a brain chemical that affects sleep patterns and mood. Its production in the brain is affected by the body’s exposure to sunlight.
- changes in the body’s biological clock. Sunlight levels increase over spring/summer months, then decrease in the fall and winter. These seasonal changes can disrupt the body’s internal clock and production of melatonin, which then disrupt our sleep and mood.
Of all cases of depression, we can best pinpoint the cause of SAD: sunlight (either too much or too little).
Probably for this reason, one of the main risk factors for SAD is living far north or south of the equator, where people have the longest summer days and shortest winter days.
Research confirms this: the risk for SAD is nearly ten times greater for Alaska residents as those who live in Florida.[1]
And the main effect of sunlight is to synchronize our internal biological clocks, producing the right brain chemicals at the right times and in the right quantities to regulate our mood and ensure that we get adequate sleep.
There also might be a role for vitamin D.[2] The body makes its own vitamin D when we get enough sun exposure, and vitamin D may help in making the brain chemicals important for regulating mood.

How to treat SAD: Let there be light
As a depressive disorder, SAD can be treated with antidepressant drugs and talk therapy, like cognitive behavioral therapy.
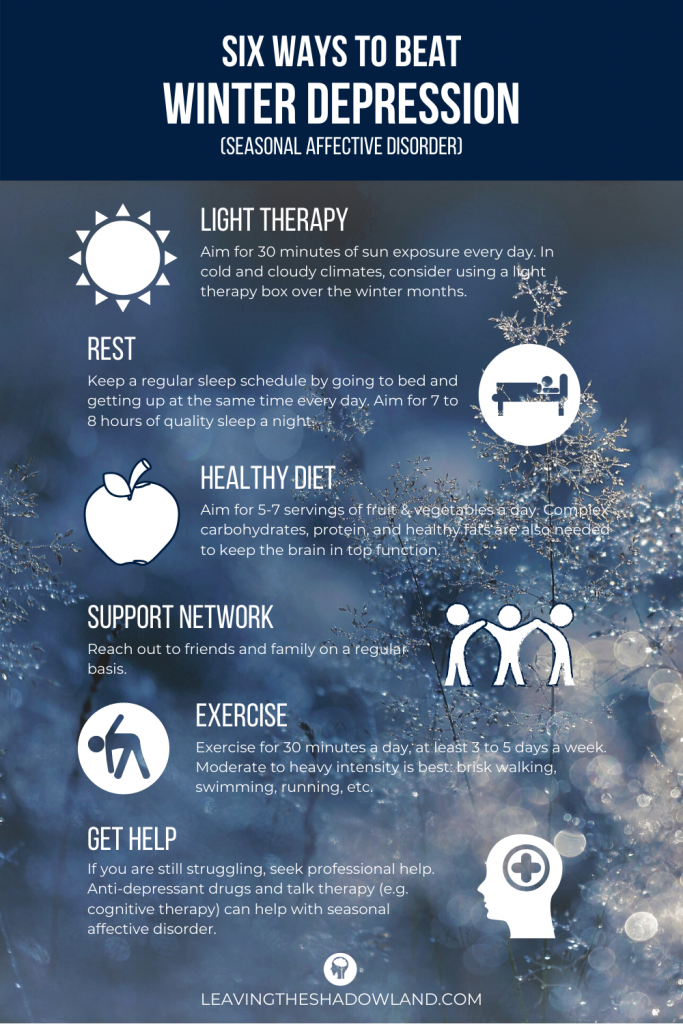
Here’s a handy, pinterest image in case you’re interested:
But getting light exposure is also key. Natural or “full-spectrum” sunlight is best, so try to get outdoors at least thirty minutes a day (you will get some light benefit even on cloudy days).
In bleak winter months, those living far from the equator can try light therapy. This involves sitting in front of a light therapy box that emits very bright light while filtering out harmful ultraviolet (UV) rays.
Here are some popular light box choices at Amazon.com
Some suggest using tanning beds as an alternative. But according to the Mayo Clinic, tanning beds are ineffective and expose the skin to cancer-causing UV light.[3]
In a recent review of several research studies of patients with both seasonal and non-seasonal depression, light therapy was found to be as effective as antidepressant drugs, and the combination of the two was even better.[4]
How to do light therapy
For winter SAD, start light therapy in the fall months when the cloudy days come. Keep doing it until sunny days return in the spring.
During each session:
- In winter months, do light therapy first thing in the morning, preferably upon waking.
- Sit close enough to the light box so that the light enters your eyes, about 16 to 24 inches (41 to 61 centimeters) away from your face. It’s not enough to get light exposure to the skin. DON’T look directly at the light, though, as this will damage your eyes.
- Use the right combination of intensity (measured in lux) and duration for the light box you are using. You should follow the manufacturer’s instructions, but here are some basic guidelines:
- For a 10,000 lux light box, daily sessions should be 20-30 minutes.
- For a 2,500 lux light box, daily sessions should be longer.
Light therapy can start to ease symptoms within a few days to a couple weeks. If your symptoms don’t improve, talk to your doctor about other treatments like medication or psychotherapy.
Cautions about Light Therapy
As always, talk to your healthcare professional before starting any kind of medical treatment.
Use extra caution if you:
- have a condition that makes you extra sensitive to light, like lupus
- take medications that make your skin sensitive to light, like some anti-inflammatory drugs, antibiotics, or the herb St. John’s Wort
- have an eye condition
Be sure to talk to your doctor first if you have bipolar disorder. Light therapy can sometimes trigger manic episodes.
Short-term side effects of light therapy include eyestrain, headaches, and nausea. They often go away on their own. If they don’t, talk to your doctor about changing up your sessions by moving farther away from the light source, taking breaks from the light, or changing the time of day you do therapy.
For more information on SAD and its treatments:
For more information about Light Therapy:
[1] https://www.nimh.nih.gov/health/topics/seasonal-affective-disorder/index.shtml
[2] Shah, J., & Gurbani, S. (2019). Association of Vitamin D Deficiency and Mood Disorders: A Systematic Review. In Vitamin D Deficiency. IntechOpen.
[3] https://www.mayoclinic.org/tests-procedures/light-therapy/about/pac-20384604
[4] Geoffroy, P. A., Schroder, C. M., Reynaud, E., & Bourgin, P. (2019). Efficacy of light therapy versus antidepressant drugs, and of the combination versus monotherapy, in major depressive episodes: a systematic review and meta-analysis. Sleep medicine reviews, 101213.
Dr. Pamela Coburn-Litvak has published research articles on exercise and stress in Neuroscience and Neurobiology of Learning and Behavior. Her latest book, Leaving the Shadowland of Stress, Anxiety, and Depression, was published in 2020.
After receiving a Ph.D. in Neurobiology and Behavior from the State University of New York at Stony Brook, she served as both Assistant Professor of Physiology & Pharmacology and Special Assistant to the Vice President for Research Affairs at Loma Linda University in Loma Linda, California. She then joined the Biology department at Andrews University and developed courses in human physiology as well as the neurobiology of mental illness. She also founded Rock @ Science LLC, a company that specializes in health and science education and web development. She co-developed the brain and body physiology segment of the Stress: Beyond Coping seminar with its creator, Dr. William “Skip” MacCarty, DMin.
Dr. Coburn-Litvak currently lives in California with her husband. Their two daughters are mostly grown and attending school elsewhere.
When she’s not studying or teaching about stress, she enjoys stress-relieving activities like puttering around the garden, taking nature walks with her family, knitting, cooking, and reading.


